This activity for Diabetic Retinopathy education is provided by Med Learning Group.
This activity is supported by an independent medical education grant from Regeneron Pharmaceuticals, Inc.
Copyright © 2019Med Learning Group. Built by Divigner. All Rights Reserved.
Diagnosis and Associated Comorbidities
Proliferative diabetic retinopathy (PDR) and diabetic macular edema (DME) can lead to significant vision loss.1 However, prevention and early recognition of diabetic retinopathy (DR) allow for timely treatment and improved visual prognosis.1,2 Unfortunately, many people with DR do not experience symptoms until the retinopathy has progressed to more advanced and severe stages, like PDR.1
Symptoms of diabetic retinopathy may include:3,4
- Decreased or fluctuating visual acuity
- Sudden vision loss
- Difficulty reading
- The appearance of “floaters”
- Changes in color perception
- Poor night vision
- Metamorphopsia
- Dark or empty areas of vision
- Progressive vision loss, especially for those not properly followed or treated
Diagnosis of PDR involves a complete eye exam, including a close examination of the iris and gonioscopy of the angle before dilation to look for neovascularization of the angle (NVA) and iris (NVI).1 A dilated exam is essential as only 50% of eyes have correctly classified retinopathy severity through undilated pupils.1 Key features of PDR include neovascularization of the disc (NVD), iris (NVI), angle (NVA), or “elsewhere” (NVE), usually along the vascular arcades; these new vessels often form at the interface between perfused and nonperfused areas of retina.2

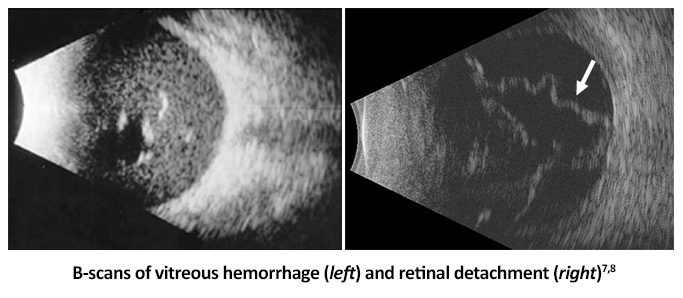
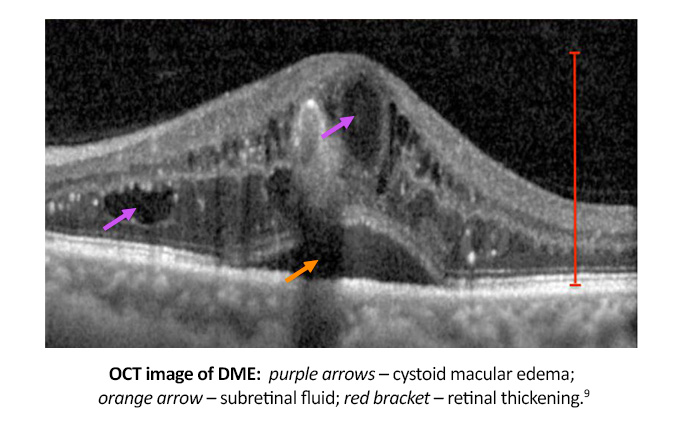
Additional testing with optical coherence tomography (OCT) or fluorescein angiography (FA) may be indicated, especially if there is a concern for diabetic macular edema (DME).3 B-scan ultrasonography can aid in the evaluation and diagnosis of an eye with vitreous hemorrhage, medial opacity, or retinal detachment.1
Once PDR is identified, some providers choose to further stratify the condition into non-high-risk and high-risk PDR. Non-high-risk PDR has almost a 50% chance of progressing to high-risk PDR in as little as a year; therefore, should be re-examined every 2-4 months.1 Eyes with high-risk PDR have an increased likelihood of vision loss and usually display neovascularization (of the optic disc or elsewhere) and vitreous/preretinal hemorrhage.1
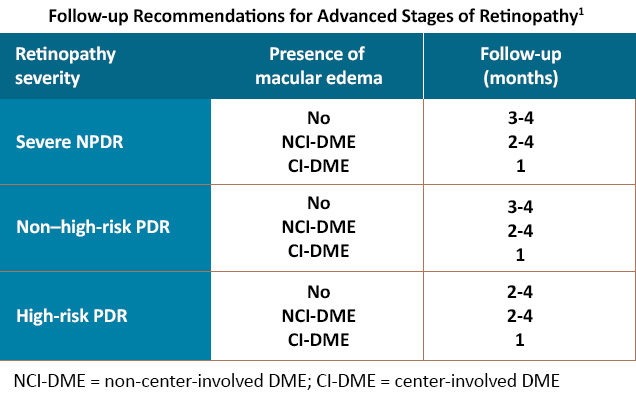
Follow-up examinations in PDR, as with nonproliferative disease, depends on the severity of DR and the presence of DME, along with individual patient factors.1
DME can occur at any stage of DR but is more commonly noted with increasing retinopathy severity.9 The natural history of DME varies, with some eyes having chronic persistent DME lasting years, while others have a quick, spontaneous resolution.9 Unfortunately, the risk of DME recurrence remains regardless of disease course, and if left untreated, can lead to significant vision loss.9
Recent guidelines classify DME into two types: center-involved (CI-)and non-center-involved (NCI-) DME.2 CI-DME is more likely to cause blurred vision and metamorphopsia and increases the risk of losing three or more lines of visual acuity.9 OCT findings of DME include retinal swelling, cystoid macular edema, and subretinal fluid.9
Like NPDR, the comorbidities associated with PDR include hypertension and hyperlipidemia.1,2 People with metabolic syndrome (a collection of risk factors that increase the risk of developing heart disease, diabetes, and stroke) have a higher risk of DR progression.1
References
- Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology. 2020;127:P66-P145.
- Wong TY, Sun J, Kawasaki R, et al. Guidelines on Diabetic Eye Care: The International Council of Ophthalmology Recommendations for Screening, Follow-up, Referral, and Treatment Based on Resource Settings. Ophthalmology. 2018;125:1608-1622.
- Gregori NZ. Diabetic Retinopathy: Causes, Symptoms, and Treatment. American Academy of Ophthalmology®. EyeSmart®. https://www.aao.org/eye-health/diseases/what-is-diabetic-retinopathy
- Columbia University. Proliferative diabetic retinopathy. https://www.columbiaeye.org/education/digital-reference-of-ophthalmology/vitreous-retina/retinal-vascular-diseases/proliferative-diabetic-retinopathy-pdr
- Retina Gallery. Gonioscopy, neovascularization in the angle. https://retinagallery.com/displayimage.php?album=917&pid=7579#top_display_media
- Bhatia L, Chen TC. Glaucoma quiz 5. Massachusetts Eye and Ear Infirmary (MEEI). 2004. https://www.djo.harvard.edu/print.php?url=/physicians/kr/680&print=1
- Strohbehn A, Sohn EH. Retinal detachment: from one medical student to another. EyeRounds. 2013. https://webeye.ophth.uiowa.edu/eyeforum/tutorials/retinal-detachment-med-students/index.htm
- The Retina Centre. Diabetic retinopathy. http://www.retinacentre.com.au/medical-retina/diabetic-retinopathy/#1488497100371-e7f77967-83c1
- Jacoba CM, Mitzner MG, Vavallerano J, et al. Diabetic Macular Edema. American Academy of Ophthalmology®. EyeWiki® Accessed May 9, 2022. https://eyewiki.org/Diabetic_Macular_Edema
All URLs accessed 5/9/22.